

Case Report
Valentina Baro
Luca Denaro
Andrea Landi
Alberto D’Amico
Nicola Bresolin
Giulia M. Furlanis
Recieved on: 2023-11-11, Accepted on: 2023-12-22, Published on: 2023-12-28
Jacobsen Syndrome is a rare genetic disease caused by partial deletion of chromosome 11 and is characterized by mental and motor delay, organs malformation and platelet dysfunction. Even if the intracranial hemorrhage is a real risk in Jacobsen Syndrome, this complication remains an event poorly described and the chronic subdural hematoma (cSDH) is an unknown entity in literature.
We reported a case of a 2-year-old female affected by Jacobsen Syndrome with sudden onset of neurological impairment secondary to a chronic subdural hematoma, resolved with a mini-craniotomy. Furthermore, we have conducted a review of the literature about intracranial hemorrhages in Jacobsen Syndrome. According to our experience, chronic subdural hematoma is a sneaky event, and we suggest taking it in account to improve management of child affected by Jacobsen Syndrome.
Jacobsen Syndrome is a genetic syndrome caused by partial deletion of chromosome 11. Its prevalence is estimated at 1/100000 births. Common features of this syndrome include psychomotor development delay, facial dysmorphism, and several type of organs malformation. The 20% of these patients die during the first 2 years of life due to congenital heart disease.
All patients with Jacobsen Syndrome also have Paris–Trousseau syndrome, a neonatal thrombocytopenia and persistent platelet dysfunction responsible for a bleeding disorder (1). Despite that, cases of intracranial hemorrhage in Jacobsen Syndrome are anecdotical and the chronic subdural hematoma (cSDH) is an un-described event still to date.
We present a 2-year-old female with Jacobsen Syndrome diagnosed at birth on basis of clinical and genetic features (1) that was admitted in the emergency room of Pediatric Department of University of Padova for new onset headache and vomit without head trauma. She had a history of complex partial epilepsy resolved completely with phenobarbital one year before her presentation to our attention.
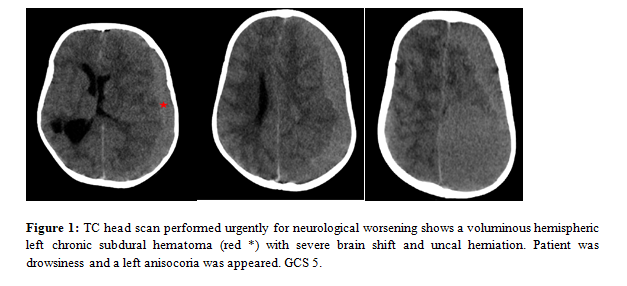
During hospitalization she presented a sudden drowsiness and a left anisocoria occurred. An urgent head CT scan showed a voluminous left chronic subdural hematoma of 4x6 centimeter in maximum diameter (DM) with important shift and initial uncal herniation. Indeed, the left chronic subdural hematoma was (2) characterized by inhomogeneous areas into hematoma as by hemorrhage in different evolutive stages. Moreover, the cerebral parenchyma presented multiple malacic areas as previous episodes of ischemic stroke (Figure 1).
A left fronto-temporal mini-craniotomy was urgently performed, and evacuation of the subdural hematoma was obtained. We have chosen to perform a mini craniotomy to ensure an optimal decompression given the shift of median structures. Furthermore, the presence of membranes in the subdural blood collection did not allow their removal through a single burr-hole. Surgery was performed after administration of platelet substitute (2). No significant brain re-expansion was observed following to surgery.
Anisocoria disappeared and no complications occurred. A post-operative head CT scan confirmed a complete evacuation of the subdural hematoma (Figure 2). After a brief period in pediatric intensive care unit (ICU) the patient was awakened, and she was dismissed to a non-intensive clinical unit for furthermore evaluations with a good recovery of neurological function.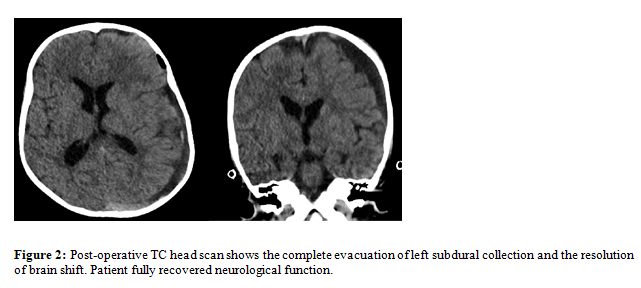
From our review of literature, knowledges about intracranial hemorrhage in Jacobsen Syndrome are sparse and the first cases have been identified by Grossfeld et al. in 2010 (2) (3) .To date, Grossfeld serie is the largest with six patients affected by Jacobsen Syndrome with different kind of brain hemorrhage. However, the cSDH is a previously unreported complication.
In our case the child with history of moderate mental retardation, seizures and a Paris–Trousseau syndrome presented an episode of vomit, following by a sudden neurological impairment caused by a voluminous left hemispheric chronic subdural hematoma with a severe mass effect and uncal herniation. Child recovered completely following a mini craniotomy and evacuation of subdural collection. Usually, the cSDH occur more frequently in geriatric population, conversely in child is an event poorly described even in case of platelet dysfunction but usually associated to cerebral atrophy, anticoagulant drugs, hematological disorder and shaken baby syndrome (4) (5) . Furthermore, in our case no head trauma was reported by family and the shaken baby syndrome was excluded.
We retain that in these patients the connecting ring between chronic subdural hematoma and his onset is the presence of cerebral atrophy and platelet disorder, features of Jacobsen Syndrome, that predisposing to repeated intracranial bleeding with possibility of the development of cSDH also without history of head trauma.
The cSDH is a sneaky and slowly process that manifests itself when the compression on the brain is such as to cause neurological impairment making this complication sudden and unpredictable. For these reasons an early diagnosis and an effective surveillance of these patients is very difficult.
In current English literature a strategy of management of intracranial bleeding in Jacobsen Syndrome is not clear and a follow up for a possible development of subdural hematoma is not a topic debated. The management of these patients should involve different professional profiles as pediatrics, neurologists, geneticists, physicians, hematologists and neurosurgeons and their treatment would require a multidisciplinary approach.
According to our experience, we suggest that a close neurological observation may be appropriate also in patients with normal neurological findings minimizing head trauma when possible and heeding new-onset and unusual headaches that should require a radiological study.
Although further studies with more case reports will be needed, we emphasize that intracranial hemorrhagic complication must be considered in management of patients affected by Jacobsen Syndrome to avoid a possible and life-threatening event and so to identify the better strategy of treatment of the disease.
Ethics approval and consent to participate: Ethics approval was not due for this study
Consent for publication: All necessary consents were collected before the publication of this manuscript
Availability of data and material: Not applicable
Competing interests & Funding: Authors declare no conflict of interests and No funding was received for this study.
Acknowledgements: None
Authors' contributions: Alberto D’Amico contributed to manuscript conceptualization and data curation; Alberto D’Amico and Nicola Bresolin and Giulia Melinda Furlanis contributed to original draft preparation, software analysis, investigation and figures preparation; Valentina Baro and Andrea Landi contributed to methodology, manuscript review and editing; Alberto D’Amico contributed to visualization and review of manuscript; Luca Denaro contributed to manuscript validation and project supervision. All authors have reviewed and agreed to the final version of the manuscript.