

Letter to Editor
Alberto D’ Amico
Valentina Baro
Giulia Melinda Furlanis
Luca Sartori
Luca Denaro
Andrea Landi
Recieved on: 2023-07-17, Accepted on: 2023-08-26, Published on: 2023-08-29
Neurofibromatosis type 2 (NF2) is a rare autosomal disorder characterized by arising of multiple lesions in several organs with different histology. For this reason, NF2 patients underwent many surgical procedures during their lifetime and spinal tumors represent an important part of them. Intradural extramedullary (IDEM) tumors amount of the two-thirds of spinal lesions. In NF2 population intradural extramedullary (IDEM) tumors are common and are a challenging entity due their tendency to be multiple, to arise in the whole of spine. Indeed, due to several procedures are needed to remove them during their lifetime neurological function as well as the spine stability could be compromised.
To date, a gross total resection remain the goal standard of treatment of IDEM tumors, and several microsurgical techniques are described. To decide which surgical approach performs and to achieve a gross total resection an accurate preoperative planning is paramount. We described a case of 19-year-old male underwent surgery for a C4 intradural extramedullary lesion performing a left unilateral approach with a tailored and a minimally invasive C4 hemilaminectomy.
Even if this approach is widely described in literature, the hemilaminectomy has not been performed before in NF2 patients.
To the best of our knowledge, a hemilaminectomy to achieve a gross total resection in NF 2 patient has not been highlighted yet. Mini invasive approach is attractive and should be encouraged in NF2 patients.
Neurofibromatosis type 2 is a neurocutaneous (NF2) syndrome, characterized by the development of several histotype tumors of whole nervous system. Intradural extramedullary tumors (IDEM) amount until to 60% of spinal lesions [1]. For this reason, multiple spinal procedures were performed during NF2 patient lifetime impacting on their long-term morbidity significantly.
We present a case of a 19-year-old male with NF2 underwent surgery for a left C4 antero-lateral intradural extramedullary lesion. This patient underwent previous multiple spinal surgery during his lifetime. The onset symptom was a progressive weakness of left deltoid muscle (MRC 4/5). A cervical MRI with contrast showed an antero-lateral egg-shaped intradural extramedullary lesion of 2 cm with contrast enhancement (Figure 1).
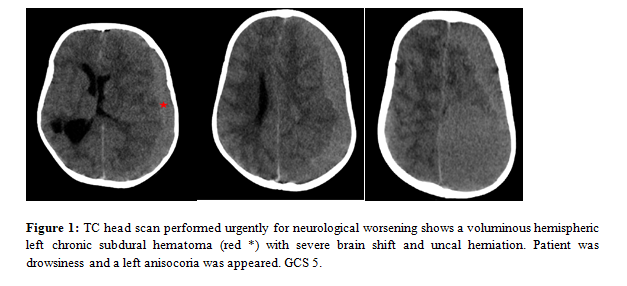
Figure 1: a) A pre-op T2-weighted cervical MRI in sagittal and c) T1-weighted with contrast in coronal plane show a C4 intradural extramedullary tumor; b)-d) Post-operative MRI T1-weighted with contrast in sagittal and coronal plane show the gross total resection of the lesion. In detail: the red arrow shows the surgical corridor through left hemilamina of C4.
Due to long surgical history of patient and to preserve his spinal stability we decided to perform a tailored C4 hemilaminectomy to remove the lesion. Surgery was guided by intraoperative neurophysiologic monitoring (IONM). No motor and somatosensory evoked potential (MEP and SEP) alterations were detected. Operative time was 160 minutes. Anatomopathological specimen confirmed the diagnosis of schwannoma (WHO I 2016). Mobilization started on the third post-operative day and patient was discharged in fifth post-operative day without cervical brace. No neck pain complained, and a good recovery of pre-operative motor deficit was obtained. At the 6-month follow up, the patient was symptom free. A cervical MRI at 12 months post-op no showed tumor recurrence or post-operative cervical kyphosis.
From our systematic review of literature about mini-invasive approach for the treatment of IDEM, 17 eligible studies described a total of 737 IDEM treated with an hemilaminectomy in adult age. 236 were meningiomas (32 %) 390 were schwannomas (53%) 127 others spinal lesion (17%). The main spinal level involved is cervical and thoracic segment, less lumbar. Data about amount of resection was mentioned in 653 cases with gross total resection achieved in 624 patients (95%) with an average of 2 levels of hemilaminectomy performed. Over the past 15 years hemilaminectomy has been widely described to obtain gross total resection in intradural extramedullary tumors. Conversely, some authors criticized the narrow surgical corridor so there isn’t accord about hemilaminectomy as first choice approach [2,3].
In current literature, while intradural spinal schwannomas are favorable to be treated with a mini-invasive approach as hemilaminectomy, meningiomas can be difficult and dangerous to remove with a unilateral approach due to their base implant, vascularization and intralesional calcification that could cause an excessive spinal cord manipulation. For these reasons several authors considerer meningiomas a very contraindication to perform hemilaminectomy [4]. Therefore, even if hemilaminectomy is a well-known approach, not is always feasible.
Turel described a decisional algorithm to perform hemilaminectomy in IDEM tumors based on numbers of lamina levels involved, type and diameter maximum of lesion. According to these authors hemilaminectomy is not convenient if more 3 levels of lamina are involved, IDEM tumors are meningiomas especially with intralesional calcification and DM is > 2 cm [5].
In accord with the authors, we performed a left hemilaminectomy of 1,5 cervical level to treat our patient obtaining a gross total resection. We increased operative field with the cut of the dentate ligament and with an intracapsular dissection of lesion to reduce spinal cord manipulation.
The use of hemilaminectomy in intradural extramedullary lesions is well-described but to the best of our knowledge, our case is the first that described use of an hemilaminectomy as minimally invasive approach for these lesions in a young NF2 patient.
The rationale to perform hemilaminectomy in NF2 population is to reduce morbidity in patients that underwent several surgeries during his lifetime to avoid long-term spinal instability respecting osteoarticular and ligamentous structures. Intact, it’s known that neurofibromatosis is an autosomal disorder characterized also by intrinsic spinal instability due to excessive ligamentous laxity. Indeed, in literature a lot of biomechanical studies described hemilaminectomy respect to laminectomy like a technique able to reduce post-operative pain and avoid spine long-term instability [6]. (Figure 2).
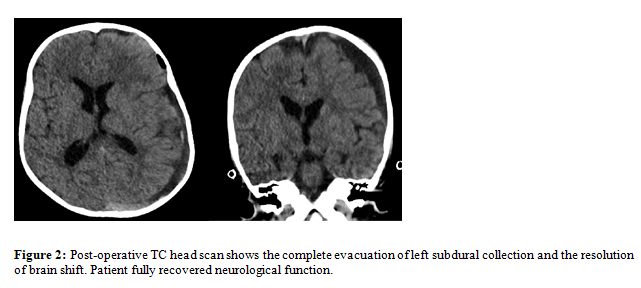
Figure 2: (a-d) Steps of hemilaminectomy of C4.
In detail: a) black arrowhead shows spinous process and supraspinous ligaments; white arrow shows C4 lamina; white arrowhead points the dura mater. b) Dura mater open. White arrows mark the C5 radicle, while the white arrowhead marks C4 radicle. Black arrows show the tumor capsule. c) Debulking of the tumor with intracapsular dissection d) Final operative field with gross total resection of tumor.
Moreover, NF2 patients are characterized by important surgery-related morbidity due to several procedures performed during their lifetime so unilateral approaches to the spinal cord should considered a valid alternative to treat intradural extramedullary lesions when possible. In our case neck pain was never complained. Early mobilization occurred and the patient was discharged on 5 post-operative day without cervical brace and in good neurological function. At follow up no cervical kyphosis was observed.
Even if the useful of hemilaminectomy in NF2 patients is still to be explored with further studies, our experience show the safety of this approach and emphasize the hemilaminectomy as mini-invasive approach to achieve gross total resection in IDEM lesion with poor morbidity and to preserve spine stability.
Ethics approval and consent to participate: Ethics approval was not due for this study
Consent for publication: All necessary consents were collected before the publication of this manuscript
Availability of data and material: Not applicable
Competing interests: Authors declare no conflict of interests
Funding: No funding was received for this study
Alberto D’Amico and Andrea Landi contributed to manuscript conceptualization and data curation; Alberto D’Amico and Giulia Melinda Furlanis contributed to original draft preparation, software analysis, investigation and figures preparation; Valentina Baro and Luca Sartori contributed to methodology, manuscript review and editing; Giulia Melinda Furlanis and Valentina Baro contributed to visualization and review of manuscript; Luca Denaro and Andrea Landi contributed to manuscript validation and project supervision. All authors have reviewed and agreed to the final version of the manuscript.
Acknowledgements: None